Glucocorticoids can have severe adverse neuropsychiatric effects, but the range and community-based population risk of such effects are unclear. In this U.K. study, researchers used a population-based general practice database to identify 370,000 patients with glucocorticoid exposure and compared them with 1.2 million patients with similar diseases (mostly asthma, lower respiratory tract infection, chronic obstructive pulmonary disease, and polymyalgia rheumatica) who had not taken glucocorticoids.
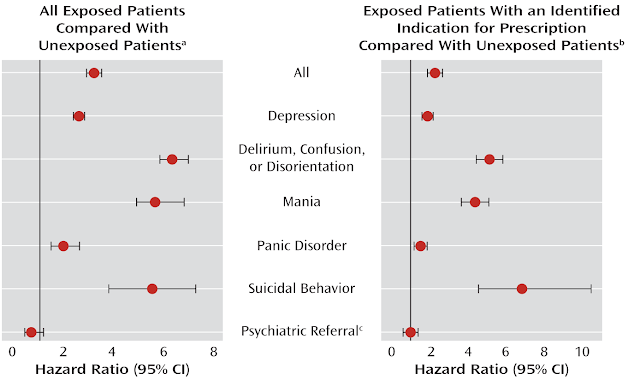
The overall incidence of any adverse neuropsychiatric effects that occurred within 3 months of a glucocorticoid prescription was 22.2 per 100 person-years of exposure. The incidence of adverse effects, adjusted for age, sex, and history of neuropsychiatric disorder, was roughly 3-fold higher for glucocorticoid recipients than for nonrecipients, ranging from roughly 4- to 6-fold higher for suicidal behavior, mania, and delirium or confusion, to about 1.5 times higher for panic disorder and depression. Incidence rose with history of neuropsychiatric disorder and with higher dosage of glucocorticoids, particularly at a prednisone equivalence of 40 mg daily.
Comment: Experienced clinicians often see these neuropsychiatric effects in patients who receive glucocorticoids for self-limited illnesses such as contact dermatitis; this study confirms such observations. Many potential confounders can affect a retrospective cohort study like this, including possible differences in patients with the seemingly same disease who are or are not prescribed glucocorticoids, but these results caution clinicians to consider these risks when prescribing glucocorticoids.
Source: Fardet L et al. Suicidal behavior and severe neuropsychiatric disorders following glucocorticoid therapy in primary care. Am J Psychiatry 2012 May 1; 169:491.


No comments:
Post a Comment